A Haunted History: The Dark Side of Mental Health Treatments in the UK
- Discovery Journal

- Sep 17, 2025
- 6 min read
Halloween is a time for haunted houses, ghost stories, and creepy costumes, but some of the scariest stories are not fiction at all. The history of mental health treatment in the UK is filled with chilling practices that would make any horror film pale in comparison. From the infamous Bedlam asylum to outdated “cures” like ice baths and bloodletting, the way people once treated mental illness shows just how far we’ve come.
Thankfully, today we live in an era where therapy, medication, and simple self-care practices like journaling offer far more humane support. But looking back at this haunted history gives us perspective and a deeper appreciation of how important compassion and understanding are in mental health care today.
The Haunted History of Mental Health Treatment in the UK:
The Horrors of Bedlam

The Bethlem Royal Hospital, nicknamed “Bedlam,” became a symbol of chaos. Established in 1247, it is one of the oldest psychiatric hospitals in the world. By the 17th century, it had gained notoriety for allowing the public to pay a penny to gawk at patients, treating people with severe mental illness as a spectacle.
Survivor accounts are rare, but we know patients were often chained, starved, or left in squalid conditions. Daniel Defoe, author of Robinson Crusoe, once described Bedlam as a place where patients “rattled their chains” for visitors’ amusement.
Patients at the Bethlem Royal Hospital (Bedlam) came from all walks of life. Records from the 17th and 18th centuries show people admitted for conditions we’d now recognise as epilepsy, postnatal depression, bipolar disorder, schizophrenia, or even alcoholism. Others were admitted for reasons that seem shocking today: poverty, homelessness, or simply being “difficult” for their families to manage.
The majority of patients in Bethlem Royal Hospital were adults, though some children as young as 10 are documented, and women and men were admitted in fairly equal numbers, though women were often labelled with vague diagnoses like “hysteria.” The strict cultural conformities of the time often meant women were more likely to be admitted without due course.
While some patients did recover and were discharged (particularly those with temporary crises or what we’d now call situational depression), many never left, either because their conditions were poorly understood or because stigma made families unwilling to take them back.
Myth of the time: People with mental illness were “possessed” or “dangerous” and therefore deserved confinement.
Reality: Many patients were ordinary people experiencing conditions like postpartum depression, epilepsy, or trauma.
💡 At least today, you don’t need chains and a gawping audience to deal with stress; the Discovery Journal is a far kinder option.
Victorian Fears and Misconceptions
The Victorian era is one of the most discussed periods in mental health history because it represents both progress and regression. On the one hand, the Madhouses Act of 1828 introduced regulations requiring inspections of asylums, and the Lunacy Act of 1845 made mental illness a public health concern rather than a private shame.
New asylums were built with the intention of being therapeutic, with gardens, work programs, and more humane care than Bedlam.
However, asylums quickly became overcrowded and underfunded. What began as a progressive step soon regressed into warehousing patients, removing them from society rather than helping them reintegrate.
Women were disproportionately affected. Victorians often pathologised normal female behaviour: “hysteria,” “nervous conditions,” or even menopause were reasons for commitment. Some husbands admitted wives simply for being disobedient or outspoken, since women had little legal recourse. This gender bias is one reason the Victorian era is still discussed so much today.
Women labelled ‘hysterical’: Many women were institutionalised for behaviour that challenged social norms, from postnatal depression to simply being outspoken.
The myth of ‘curing madness with marriage’: Doctors sometimes suggested that marriage or pregnancy could “stabilise” women deemed unstable.
Restraint chairs: Some asylums used “tranquilliser chairs” to strap patients down for hours, believing it would calm their minds.
Personal accounts from asylum records reveal stories like that of Elizabeth Packard, wrongly committed by her husband in 1860 after disagreeing with his religious views. Though American, her case mirrors many UK women’s experiences at the time. She later became a fierce campaigner for patient rights.
💡 Victorians thought marriage could cure hysteria. We’d recommend journaling instead.
Outdated Treatments That Seem Like Torture
Some of the so-called “treatments” for mental illness in history sound more like torture devices than medical care. While most have thankfully been abandoned, a few evolved into safer, evidence-based therapies we still recognise today.
Bloodletting and purging: Common in the 17th and 18th centuries, doctors believed mental illness was caused by an imbalance of bodily fluids. The “solution” was draining blood or inducing vomiting — treatments that weakened rather than healed.
Ice baths and cold water dunking: Patients were plunged into freezing water in the hope of shocking them “back to their senses.”
Straightjackets and confinement: Restraint was often used as a substitute for treatment, keeping patients locked away rather than addressing the cause of their distress.
Rotational therapy: Patients were strapped to chairs and spun rapidly, under the belief this would “reset” the brain. Many vomited or passed out.
Do Any Still Exist Today?
Many of the most terrifying treatments are thankfully gone. But a few evolved into more humane practices:
Electroconvulsive Therapy (ECT): Early versions were traumatising and unregulated, but modern ECT (done under anaesthesia and controlled doses) is still used today to treat severe depression.
Cold water immersion: Once used as punishment, this has echoes in today’s interest in cold water therapy for anxiety or inflammation, though the modern practice is voluntary, safe, and evidence-based.
Straightjackets: Now replaced by far stricter rules on physical restraint in mental health care.
Did they ever work? Sometimes, but usually by accident. For example, cold water shocks occasionally calmed agitated patients, but the trauma outweighed the benefit. Bloodletting occasionally reduced fevers linked to infections but did nothing for mental illness.
As for the doctors, they were often respected, but within the wider medical community, many were considered fringe practitioners, as psychiatry was not yet a fully established discipline. Some, like Dr. John Connolly, advocated reform and humane care, but others were more aligned with showmanship and pseudo-science.
💡 Prefer your mental health routine without ice baths and spinning chairs? Try the Discovery Journal!
The Lobotomy Era

Introduced in the 1930s, the lobotomy was based on the theory that mental illness was caused by faulty connections in the brain. Portuguese neurologist António Egas Moniz, who pioneered the procedure, believed severing those connections in the prefrontal cortex could “reset” the mind.
At first, results seemed promising. Some patients appeared calmer, less anxious, or less aggressive after lobotomies, but at a terrible cost. Many were left emotionally blunted, cognitively impaired, or permanently disabled.
Doctors were drawn to lobotomies in part because there were so few alternatives at the time. Psychotropic medications (like antidepressants and antipsychotics) didn’t exist yet, and overcrowded asylums desperately wanted a “cure.” Moniz was even awarded the Nobel Prize in 1949 for his work, which lent credibility to the procedure.
Today, lobotomies are considered one of the darkest chapters in mental health history, a reminder of how desperation and lack of understanding can lead to disastrous medical practices. While lobotomies were more common in the US, the UK also adopted the practice before it was eventually abandoned, and by the 1970s, the practice was largely abandoned, replaced by medication and psychotherapy.
Mental health myth of the time: Mental illness could be “cut out.”
Reality: Complex emotional and neurological conditions cannot be solved with a scalpel.
💡 Lobotomies were once seen as cutting-edge. We’d say writing in the Discovery Journal is a sharper idea.
From Horror to Healing
The good news? We are no longer in this dark era. Today, mental health care in the UK emphasises therapy, community support, and accessible tools for self-reflection. Practices like journaling are now recognised as safe, effective ways to manage anxiety, depression, and stress.
This is where tools like the Discovery Journal come in. Unlike the haunted methods of the past, guided journals offer a safe, modern, and effective way to support mental health. Instead of fear or punishment, they encourage reflection, self-expression, and growth. With prompts that gently guide you, journaling helps make sense of emotions that might otherwise feel overwhelming, making your mental health journey far more manageable and much less frightening.
And it’s not just anecdotal. Research has shown that expressive writing and guided journaling can reduce symptoms of anxiety and depression, improve mood, and even strengthen immune function. Studies from the University of Texas found that people who journal regularly reported better emotional regulation and fewer stress-related visits to the doctor. What’s even more powerful is that these benefits don’t require hours of effort; just a few minutes a day can make a difference.
By building reflection into your routine, the Discovery Journal turns journaling into a sustainable practice. Where once people were subjected to harsh treatments with little hope of recovery, we now have simple, compassionate tools that put control back in your hands.
Forget ice baths and bloodletting, try the Discovery Journal instead.
The haunted history of mental health treatment in the UK is grim, but it reminds us how important progress is. We’ve moved from punishment and fear to compassion and science. This Halloween, as you enjoy your ghost stories, remember that some of the darkest tales are real but so is our ability to change.
$14.99
Beginners Journal
Product Details goes here with the simple product description and more information can be seen by clicking the see more button. Product Details goes here with the simple product description and more information can be seen by clicking the see more button
$32.99
Discovery Journal - Brown
Product Details goes here with the simple product description and more information can be seen by clicking the see more button. Product Details goes here with the simple product description and more information can be seen by clicking the see more button
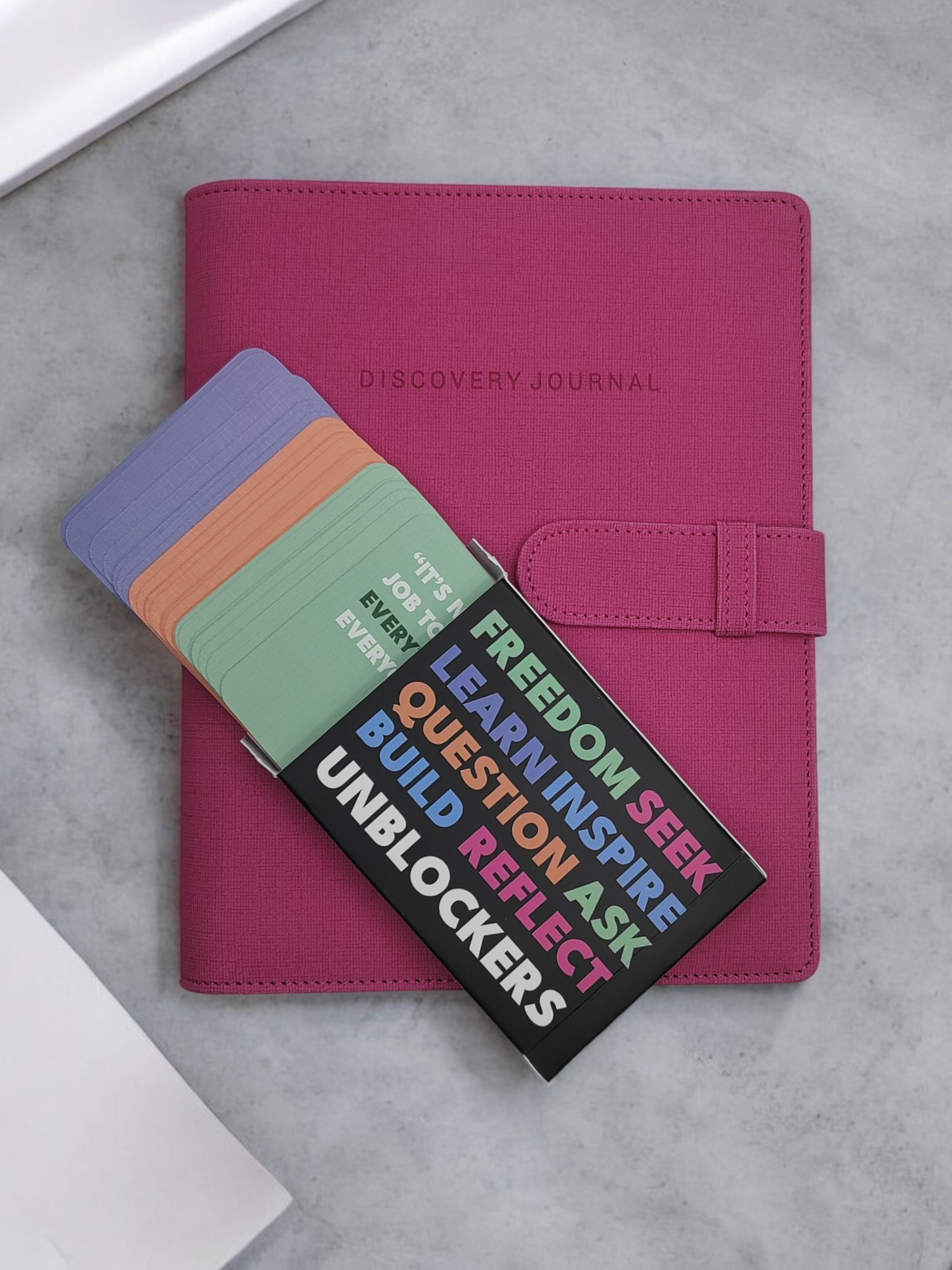
$31.00
Aspiring Author Pack
Product Details goes here with the simple product description and more information can be seen by clicking the see more button. Product Details goes here with the simple product description and more information can be seen by clicking the see more button




Comments